The benefits and drawbacks of intranasally-delivered medications
The drug development pipeline in psychiatry is running dry with few novel treatments on the horizon. Despite the increasing incidence of psychiatric illnesses worldwide, pharmaceutical companies are spending less on developing treatments for these disorders.
One of the main reasons for this slowdown is the lower chance of a novel psychiatric drug eventually reaching the market compared to other illness categories.
The development of new drugs isn’t cheap – it takes around 15 years and US$800 million to bring a new medication to market. Instead of spending shrinking resources on developing new psychiatric medications, it’s much cheaper to repurpose medications that have already in use for other purposes.
Less resources and time are needed to test the safety of these medications as this this groundwork has been largely done. More importantly, this development approach benefits the patient as it can accelerate the time taken for medications to reach the market.
There are two main approaches for drug repurposing: using a medication that has been approved for other illnesses or using a new drug administration method for an existing treatment.
In our paper published in Molecular Psychiatry, we describe the promise and pitfalls of administering psychiatric medications through the nose (preprint available here if you can’t access the journal).
The benefits of intranasal administration
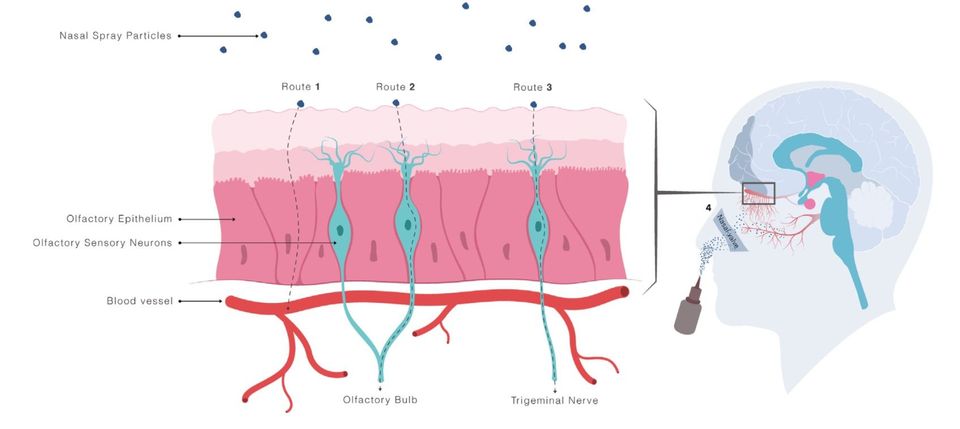
Intranasal administration is thought to provide direct central nervous system (CNS) access via trigeminal and olfactory nerve fibre pathways. These nerve fibres innervate the upper and posterior areas of the nasal cavity and access the brain through small gaps in the skull.
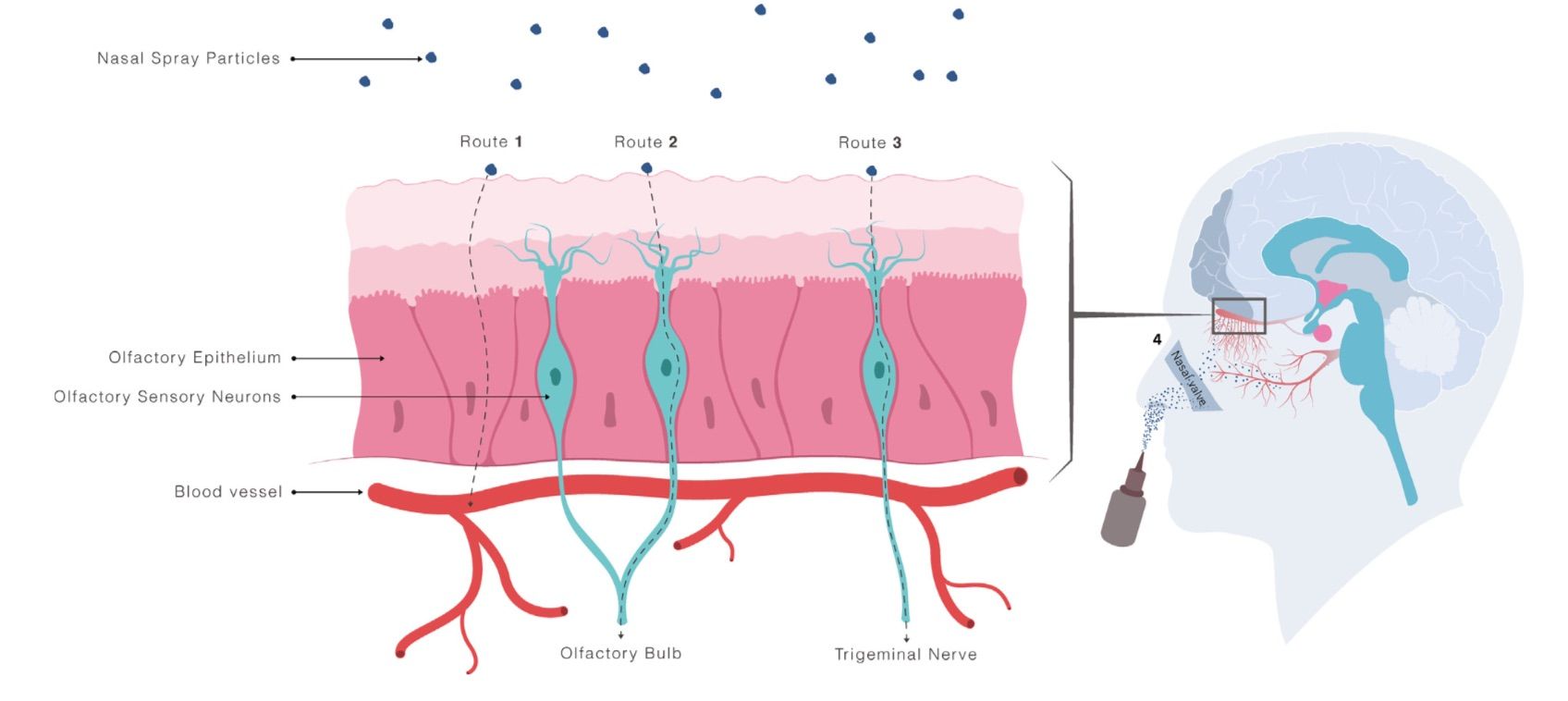
Another reason by intranasal administration is attractive is that the nasal cavity is the only accessible surface on your body that has direct access to the central nervous system
Transport to the brain via these nerve fibres provide a route that can circumvent the blood-brain barrier, which is a formidable obstacle for systemically administered drugs (especially larger drug molecules) to enter the brain.
It may also provide a safer means of administering medications in emergency situations where intravenous or intramuscular administration could present danger to both medical staff and the patient due to potential needle-stick injury. When it comes to self-administration of medication, people understandably prefer nasal administration to injections so this new method may also improve adherence.
To date, there have been 21 registered clinical trials that have investigated the intranasal administration of a psychopharmacological agent, with the majority assessing oxytocin treatment.
Making old medications new again
Oxytocin nasal spray is currently approved in many countries to assist mothers in breastfeeding by increasing milk flow. It is also commonly administered intravenously to help facilitate childbirth.
While the nursing and birthing effects of oxytocin have been known for some time, more recent research has shown that the oxytocin system is also involved in social behavior and cognition. For instance, a single nasal spray of oxytocin has been shown to increase emotion recognition. A recently reported clinical trial also demonstrates that long-term treatment improves parent-reported social behavior in children with autism spectrum conditions (ASC).
Another promising candidate for drug repurposing for psychiatry is ketamine, which is currently used for sedation. Early research has shown that intranasal ketamine reduces depression symptoms, with few side-effects.
While some trials of intranasal oxytocin and ketamine have shown promising effects, others have failed to match these results. There are three main considerations when administering CNS-targeted nasal medications that may have contributed to these mixed outcomes.
1. The exact delivery routes between the nose and brain are unclear
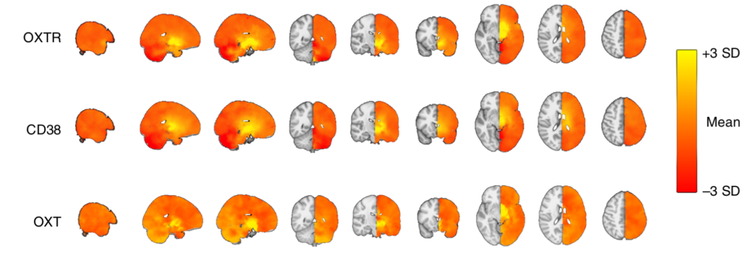
The behavioral effects of intranasally administered medications are fairly clear. However, we don’t know how these molecules get from the nasal cavity to the brain. Tracking radiolabeled molecules after nasal administration in animals has shown increased radioactivity in the CNS and the trigeminal and olfactory nerve fibres, demonstrating that intranasally administered molecules can reach the brain using these direct routes. Nevertheless, this kind of work hasn’t been done in humans before — but researchers are working on it.
We’ve also shown that intranasal (but not intravenous) oxytocin changes how we perceive emotions — but this is the only double-blind study to compare intranasal administration with another administration route, so more work is obviously required. But without radiolabeling nasally administered oxytocin, we can’t be sure how its reaching the brain to exert its effects.
2. Nasal physiology plays an important role in nasal drug delivery
The target for efficient nose-to-brain drug delivery lies deep in the nasal cavity. But to reach this target, intranasally administered medication needs to navigate past the nasal valve region.
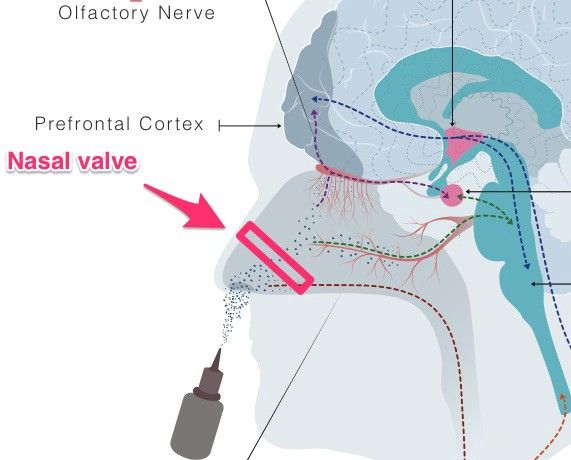
The nasal valve region — just past the reach of your finger — is the narrowest section of the nasal cavity. As nasal cavity dimensions vary from person-to-person (depending on nasal congestion), it’s no surprise that some people don’t respond to intranasal medication.
We recently measured nasal cavity dimensions before intranasal oxytocin administration and found stronger effects in people with wider nasal valve dimensions, suggesting improved delivery to key nose-to-brain sites in the upper sections of the nasal cavity.
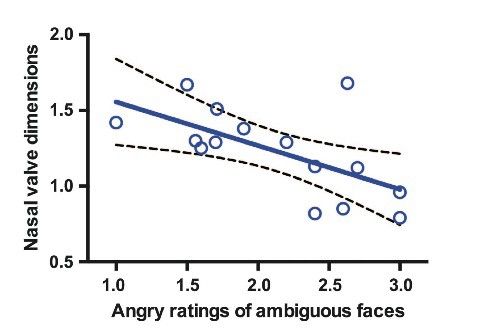
While this result highlights the need to assess nasal cavity conditions before intranasal administration, very few studies include this step in their experimental methods. Giving a brain-targeted nasal spray medication to someone with nasal obstruction is like prescribing a tablet to someone who can’t swallow — the drug can’t reach its target.
At the very least, nasal cavity health should be assessed with a basic questionnaire. However, the best approach is to measure nasal cavity dimensions using acoustic rhinometry.
An acoustic rhinometry device measures sound pulse reflections to calculate millimeter-accurate measures of nasal cavity dimensions. Measurement only takes a few minutes and the devices are fairly straightforward to use.
3. There’s less dosing control
In comparison to intravenous and oral administration, there’s less dosing control with intranasal administration.
Sniffing during administration (which is a common response) can reduce treatment efficacy as this draws the medication along the floor of the nose into the throat and gastrointestinal system, which misses the nose-to-brain transfer target in the upper areas of the nasal cavity.
In fact, the pump-actuated nasal spray devices used to deliver most intranasal medications were never designed to deliver drugs to the CNS. Their original design was use to deliver medications, such as decongestants, to the nasal cavity.
The future of intranasal administration
There’s no shortage of intranasal medication studies in psychiatry and psychology, with many of these demonstrating promising effects. Instead of adding to the growing catalogue of the intranasal medication effects, research should pivot to better understanding these effects.
By getting a better grasp on how these medications work, scientists can improve the reliability and efficacy of nasal spray medications by modifying delivery methods.